Connects
Facilitating Pharmacist - Patient Communication during COVID-19
With COVID-19 drastically altering the healthcare experience and removing human interaction, Connects, a service design solution, aims to facilitate clear communication and aid patient understanding around their medication through remote means
Collaborator: RCSI PhD Research Team | Length: 12 Weeks | Role: Lead Interaction Designer | Focus: Service Design, Design Research, UX & UI Design
The Challenge
HMW remotely facilitate and support communication between healthcare provider and patient to prevent medication error and enhance safety?
The Problem
COVID-19 rapidly altered many traditional systems and services around the world. Moving them from a physical space to predominantly digital. The healthcare system was no different, with digital care services being rapidly introduced in Ireland and across the world in order to facilitate the continued delivery of care. Although good at preventing the spread of the virus, their hasty introduction left many healthcare providers unequipped to deal with the challenges and limitations this change in service delivery would bring. As well as many patients excluded from their health care journey, threatening patient safety and increasing the risk of medication error.
The Approach
DISCOVER
DEFINE
DEVELOP
DELIVER
DISCOVER
Secondary Research — Interviews — Ethnographic Studies
Research
Why? To gain an understanding of how healthcare providers are reacting and adapting in response to COVID-19
Secondary Research
The discovery phase of this project began with desk based secondary research. This research was carried out in order to gain a base understanding of how the healthcare sector was reacting and adapting in response to COVID-19, to investigate techniques being utilised to replace touch as well as to explore standout services around the world that are addressing similar problems such as patient understanding and communication.
Primary Research
Interviews
10 interviews with patients, pharmacists, pharmacy students, members of the IPU (Irish Pharmacy Union) and nurses where carried out in order to gain insight into the current state of practice, the changes in service delivery pre and post pandemic within pharmacies, the issues associated with remote care interactions and work arounds being utilised to combat these new found challenges.
Ethnographic Research Studies
Along side conducting interviews, I carried out two guerrilla style ethnographic research studies in order to personally observe and experience the challenges being faced by patients. These studies consisted of multiple pharmacy visits as well as a digital GP consultation in order to evaluate how the removal of physical face to face interaction has impacted ones healthcare journey and understanding.
Secondary Research
Ethnographic Research Mapping
Primary Research
DEFINE
Affinity Mapping — Journey Mapping — Defining Focus
Affinity Mapping
Why? To begin thematically organising the findings, identifying problems and generating insights
The method of affinity mapping was used to begin organising the mass amount of findings into themes, allowing key problems to become apparent and insights to be drawn.
The Key Insights
01 Patient and pharmacist require a clear method of communication in order to explain, understand and question medication usage
02 Phone calls are an uncomfortable method of communication that threaten patient understanding and privacy
03 Patients tend not to retain all the instructions given, especially by phone. As a result a clear method of referral is needed
04Technology has removed patients from their healthcare journey. In order to build understanding and play a role in their health patients need to be reintroduced
05 Health illiteracy is an issue. Building a patients understanding and knowledge relies on patient level information
06 Facial expressions tell all. With the introduction of phone based care pharmacists have no method of gauging a patients understanding
07 Pharmacy resources and software are not connected. Pharmacists must jump between platforms during their work flow
08 Pharmacist’s and GP’s communicate primarily through the phone. This is not efficient. Pharmacists require a quick method of retrieving necessary patient information in order to aid safe prescribing
Journey Mapping
Why? To visually unravel the current patient experience and identify the points of contention
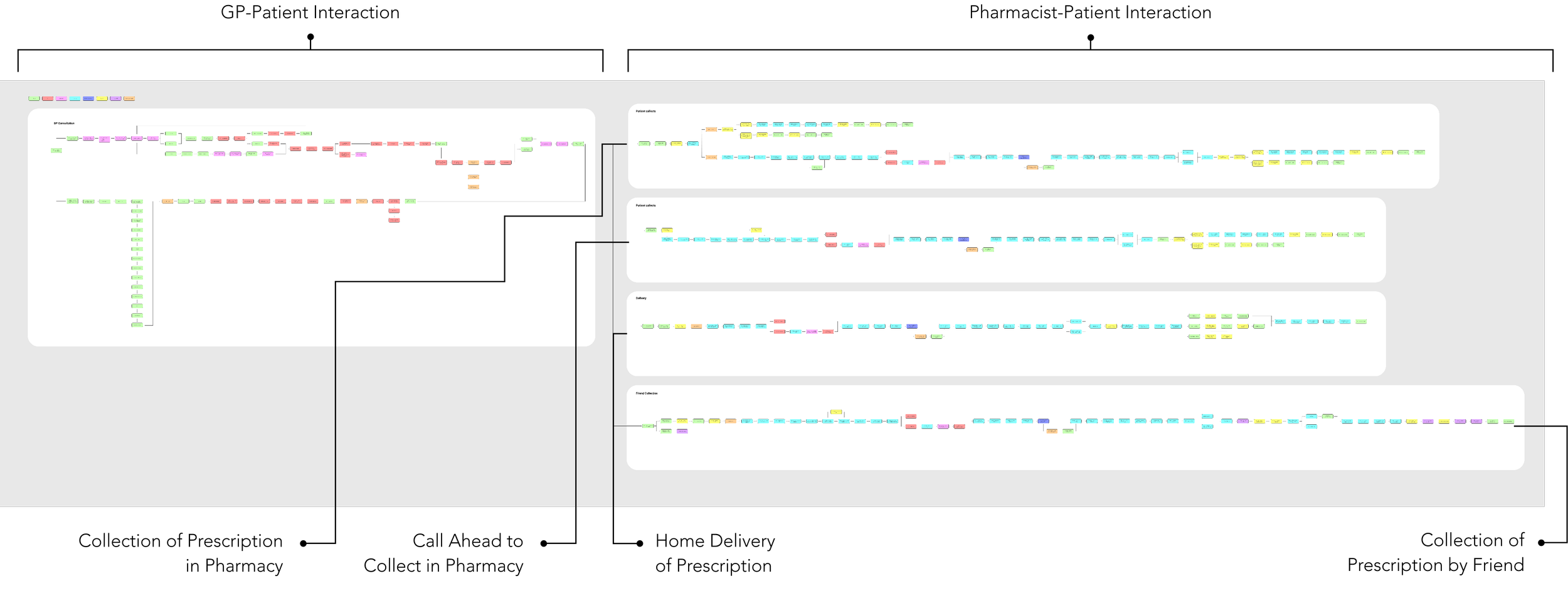
Once the key insights had been identified through affinity mapping it became apparent that in order to fully understand the complexities of this problem and initiate meaningful change I needed to visually map out the ‘as is’ process from beginning to end. Encapsulating every step from the GP-patient consultation, to pharmacy engagement, to the patient being at home with their medication.
This process enabled me to visualise each step, the multiple pain points and where interventions could potentially be integrated. However above all else, it confirmed that the service was long and the problems countless. Any devised solution could span in multiple directions and in order to make an impact I needed to hone in on a segment where the greatest need existed.
Through further analysis and user consultation the segment identified as requiring the greatest transformation was the patient-pharmacist interaction but more specifically when the prescription was being delivered or collected by a friend. This is due to the face to face interaction being replaced by a phone call or removed entirely, altering the normal delivery of information, threatening patient safety and understanding around medication.
Entire Journey
Focused Journey
Pain Points
The handwritten documentation of prescription collection and/or delivery details is a challenge due to accuracy and potential loss of information
A lack of centralised Patient Medical Records threatens patient safety if medication is prescribed without consulting the GP or patient directly
Printed medication leaflets are text heavy, inconsistent and not supporting patient level information sharing
The delivery or collection of prescriptions removes the certainty that the correct patient received the medication
Pharmacists often forget to call patients for a consultation on medication use due to the change in service delivery
The communication of instructions over the phone removes the ability to gauge patient understanding
Patients have no time to reflect and ask questions or point of reference to ease uncertainty
Defining the User
Why? To focus and ensure I am designing with my users needs in mind
The process of journey mapping made evident that the change in service delivery presented many problems. However it also made evident that these problems were not an obstacle or safety issue for all but only those that required considerable care, poly-pharmacy patients.
Poly pharmacy patients are patients on multiple medications. This means they require extensive consultation to gain a clear understanding of their medication regimes. Due to the introduction of phone based service delivery this level of care has been greatly impacted, threatening patient understanding and increasing the risk of medication error.
The development in understanding made evident that this was the user that needed designing for.
DEVELOP
Concept Development — Prototyping
Concept Development
Why? To develop a concept that holistically addresses the problem
The development stage was all about ideation and concept generation within the defined focus area, to develop a solution that holistically addressed the problems identified. Through sketching and ideation sessions multiple solutions were developed. The solutions ranged from entirely digital services to interventions that focused solely on the micro interactions. With each solution targeting different aspects of the journey. This rapid ideation process enabled me to focus in on the part of the journey that required the most attention, patient consultation, as well as consider the existing service, the user and the feasibility of the solutions being created.
The solution selected to develop further focused on facilitating remote patient consultation. A major point of potential error due to phone based consults and an inability to monitor patient adherence. By integrating new physical and digital interventions across the pharmacy preparation and patient consultation stages, this service solution aims to support pharmacists in the delivery of remote care but more importantly help patients understand how to take their medication correctly at home.
‘To be’ High Level Journey
Interventions
Redesigned Medication label using patient level language and a clean layout to aid understanding
A Numbered Pill card to act as a reference point during and after remote consultations
Numbered Stickers to link the medication box to the pill card to the medications function
A vibrant consult sticker sealing the medication bag to alert patients to initiate a phone consult
Pharmacist communication guidelines to ensure instructions are given effectively during a phone consult
An patient level online medical directory to provide patients with information on their medication
Prototyping
Why? To rapidly refine and validate the solution with users
Low-Fi Prototyping
Mid-Fi Prototyping
High-Fi Prototyping
The prototyping stage of this project was rapid but complex moving from low fidelity to high fidelity across three round of user testing, that took the form of experience prototyping, usability testing and expert evaluation in order to gain maximum user input.
Multiple adjustments were made at each stage, guided by user consultation, to inform the final solution.
DELIVER
Visual Design System — The Solution — Learnings
Visual Design System
Why? To establish standards and ensure visual consistency throughout the service solution
The visual direction of the service solution was sparked after the first round of high fidelity testing. By gaining this user feedback it became evident that the design needed to focus less on visuals and more on the clear delivery of information. As a result, the focus was on utilising a clear typeface, white space, a secondary colour palette and icons.
The Solution
01 Consult Sticker
What this project aimed to do
COVID-19 both positively and negatively altered the way people access and use medication. This project sought to uncover how these changes, brought about by COVID-19, impacted medication safety in order to form a solution to address them.
What the main problems were
The altering of the healthcare experience presented many problems. However the main limitations associated with the delivery of remote care were: patient exclusion, over reliance on verbal communication with no visual aids, an inability to gauge patient understanding, unfriendly patient resources and poor communication.
The solution
The solution developed is the altering of the GP- Pharmacy prescription service for high risk and/or poly pharmacy patients, with specific focus on the patient consultation, in order to facilitate clear communication and aid patient understanding around their medication. Designing for health is complex and comes with mass limitations and legal boundaries. As a result the service solution developed does not change existing softwares or threaten legal requirements but builds upon them.
02 Medication Labels
03 Numbered Stickers
04 Pill Card
05 Medical Directory Web App
Previous
Next